Patient-clinician relationships are vital to making shared decisions on patient care. However, it can be difficult to build these crucial connections when clinicians’ time is scarce — and when each patient interaction lasts only minutes.
While it may be challenging to implement patient-centered communication at your healthcare organization, doing so can improve a patient’s experience and lead to better health outcomes. Here’s how implementing healthcare technology can help your care team and patients communicate more effectively.
Why is it essential to improve patient communication?
Everything from obtaining a patient’s medical history to explaining a treatment plan requires clinicians to have strong communication skills and build a trusting relationship with their patients. However, most patients feel that their clinicians could improve communication with them.
Although 75% of surgeons believe they communicate well with their patients, only 21% of their patients feel they receive satisfactory levels of communication.
That same literature review explores the barriers to improved patient communication. Common issues include decreased communication skills on the provider side, lack of information, and patient resistance. These barriers can contribute to patient noncompliance with care plans, miscommunications or misunderstandings, and lower satisfaction rates for providers and patients.
It’s important to remember that nonverbal communication is often just as important as the spoken word. Clinicians need to pick up on nonverbal cues to dig deeper into patients’ expectations and needs. Similarly, patients will need nonverbal reassurance that their care team is willing to listen and values their opinions.
Offering compassion
Patients are, first and foremost, people with real emotions. The connection between patients and their providers empowers both sides to co-create treatment plans. Clinicians must listen to patient concerns, provide comfort, and build trust to give a wholly therapeutic service — especially during the COVID-19 pandemic. Quality healthcare will suffer if these basic human needs are not met first.
Patients should be encouraged to ask questions without time constraints; it’s crucial to include them in decision-making throughout their care. It’s also important to remember that not all patients come with an extensive network of family members or friends, and those who do not might need extra emotional support.
Clinicians should always be ready to deliver news — both good and bad — with compassion. Ideally, healthcare providers should validate emotions, help patients comprehend their condition, ensure patients are compliant in their treatment, and keep anxiety levels low.
Building rapport
Building rapport also leads to better patient outcomes. Improved patient communication can pave the way for symptom resolution, pain management, natural blood pressure level regulation, and beyond. When proper rapport is developed between the two parties, communication becomes a truly reciprocal, two-way exchange of information.
Forging a solid patient-physician relationship is key to helping patients let their guard down enough to open up and share critical details. Patients may hold back vital medical information if they are not comfortable with their physician. However, when the patient shares their complete health history, physicians are empowered to help patients move toward positive clinical outcomes. This kind of knowledge helps care teams deliver patient-centered care.
Four strategies to improve patient communication
Use the following methods to improve patient communication at your healthcare organization. You are bound to see improved systems that everyone — clinicians and patients alike — can get behind.
1. Nurture the provider-patient relationship
There must be a sense of trust between clinicians and their patients. To foster that trust, healthcare professionals at your practice can adopt the BATHE method. Here are a few key points to keep in mind during an appointment to foster doctor-patient communication:
- Be curious about their background: Have patients explain what they think is happening to provide context around the visit.
- Check with them first: Have patients convey how it makes them feel to develop a personal rapport. Ask open-ended questions and let them express themselves.
- How it affects them: Have patients explain what bothers them most about their healthcare troubles to identify the condition’s impact on the patient’s quality of life.
- Ask about prior care: Have patients explain how they’ve been handling the issue thus far to understand what steps their patients have already taken. Consider all treatment options.
- Empathy, first and foremost: Respond to the patient’s experience with kindness to show compassion and understanding — especially when delivering bad news.
- Make communication easy: Provide multiple channels for effective communication with your patients — whether it’s SMS, email, chat, video calls, or a patient portal. More options for communication means patients have more ways to get in touch and create a proactive relationship.
- Automate external touchpoints: Create a plan for how frequently you’ll be in touch. Even if it’s less personal, make sure you’re communicating with patients regularly — set a one-month, three-month, or six-month check-in. Send out follow-up reminders, best practices, or even just a friendly “hello.” Keep your patients engaged.
- Automate internal touchpoints: Patient filled out an assessment indicating they’re suffering from unrest at home? Automate a notification to your team so they can reach out immediately. Does the patient log an above-average A1C reading? Reach out.
All the while, clinicians should be making eye contact with the patient, whether in person or via a telehealth device. They should also exchange pleasantries, be aware of their body language and facial expressions, and listen without interrupting.
It’s important to assure patients that the staff caring for them is highly experienced without taking an overly authoritative approach. Practices where patients were made to feel empowered by their healthcare provider — rather than feeling as though their clinician assumed a patriarchal role — had as much as twice the patient retention rate.
Ask patients for regular feedback to get a solid idea of how your staff is doing with their journey toward patient-centered communication. As a clinician, you should never be afraid to ask your peers to critique your communication techniques.
Don’t forget to identify communication roadblocks specific to physicians, the patient’s demographic, and your healthcare organization’s region. For example, immigrant patients who do not speak fluent English may not fully understand what is communicated to them. This could potentially hurt their ability to voice concerns or properly follow their treatment plan.
Additionally, look for gaps in patient communication and patient satisfaction, and adjust where needed. Reports of patient-generated health data and customer feedback can give you a bird’s-eye view of where improvements need to be made. A robust Care Management platform can ensure you have all the health information you need in one place, accessed by any part of the care team that requires it — wherever and whenever they need it.
2. Educate patients
Americans are increasingly searching the internet for health resources, but they may be met with less-than-ideal readability and clarity. This presents an opportunity for care teams to help patients understand their condition and learn more.
When in doubt, provide a range of medical education resources such as reading materials, take-home handouts, studies, support groups, and helpful websites. It’s also critical to guide patients to materials that can help them understand and act on the information provided.
A good rule of thumb is to make sure the information you recommend to patients is at an approximate 5th-grade comprehension level. It will significantly increase the odds that everyone from your broad audience will understand the information you provide. When materials go above a 6th-grade level, you cannot be sure that the average American will know what to do with them.
This can quickly become confusing or even unsafe. Patients who cannot understand what you are prescribing — medication or otherwise — may not correctly follow their treatment protocols or understand when there is a problem.
3. Improve internal communication
Internal communication is just as important as communication with the patient, as they frequently go hand in hand. If internal communication is poor, challenges in patient communication often follow — as well as poor patient care.
It’s no wonder that Medical Economics reports that 96% of healthcare executives say poor internal communication leads to mistakes, and two-thirds of healthcare employees say their colleagues could help improve that.
It is wise to invest in continuing education for clinicians and your entire staff on good communication skills. A well-trained team of receptionists, nurses, and other healthcare providers will help build patient trust and relay vital patient information to the necessary team members before they even step into the exam room.
Implementing a system that helps all patient-facing employees share their knowledge with one another and do their jobs more efficiently can reduce errors due to miscommunication. With this structured approach, supported by technology, it’s clear who owns each step of a patient’s treatment plan. In addition, peers can quickly review care plans to assess quality, and tools can be implemented to measure quality improvement initiatives.
Downtime, patient dissatisfaction, and even lawsuits can be avoided with the right processes in place and the right platform. We will get into this next.
4. Use purpose-built technology
Patients appreciate when their healthcare providers are clear, direct, and make things simple for them. They don’t want to chase their clinician down to get their questions answered. If doctor-patient communication over the phone isn’t effective, you can try secure email, instant messaging, or automatic notifications to guide patients through their next steps. Just be sure you aren’t hindering patient communication and decision-making by forcing them navigate a multitude of different platforms.
Be willing to reach patients through their preferred communication methods. Newsletters and social media are great ways to create additional touchpoints with patients. In this digital era, taking advantage of the most popular communication channels shows patients that you genuinely care about keeping them informed, both during visits and in between.
Care Management software can also be used to create a revitalized sense of efficiency and ensure your patients get the treatment they need from the appropriate people at the right time. Your clinicians will be able to deliver higher quality, individualized, patient-centered care without adding to their burden or taking up their time. If your care team hasn’t spent enough time focusing on actual care delivery that prioritizes patients, you may be dealing with ineffective software. It’s time for a change.
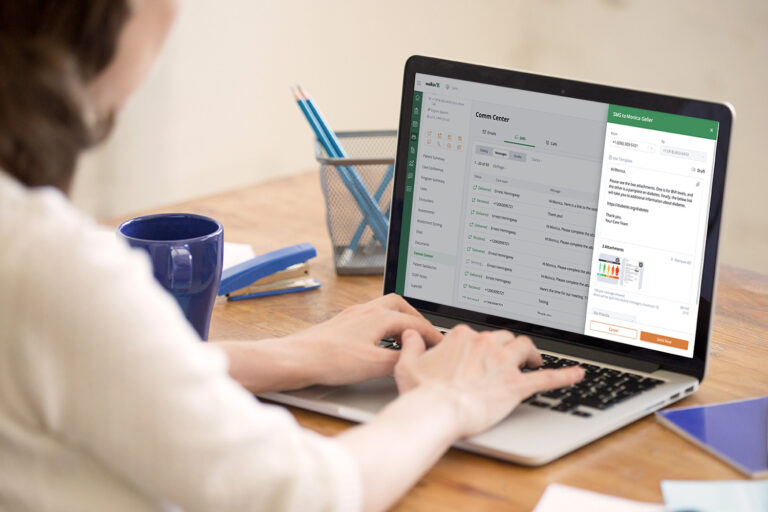
The best program will offer everything you need in one place to streamline both internal and patient communication. Care Management platforms like Welkin keep your team on track with a convenient and powerful set of applications and functions.
If you’re a program director, you need to read this.
Welkin gives you meaningful insights to inform each choice you make throughout your day at work to provide better programs. With this cutting-edge technology, you can see the bigger picture, creating a centralized space for internal staff conversations. Keep data visible, become more organized, automate processes, consolidate tools, and always stay on top of program health with data-driven decisions.
Give the team at your healthcare organization a true advantage by presenting a better system. Ultimately, you will see healthier, happier patients and more fulfilled clinical workers by leveling up your patient communication. Leaving outdated communication approaches behind will offer patients an enhanced quality of service that builds loyalty with your healthcare organization.
Learn all there is to know about improving the patient experience to begin making your program more care-centric today!