Remote Patient Monitoring
Manage your program and track your eligible reimbursements
How Welkin is relevant to RPM
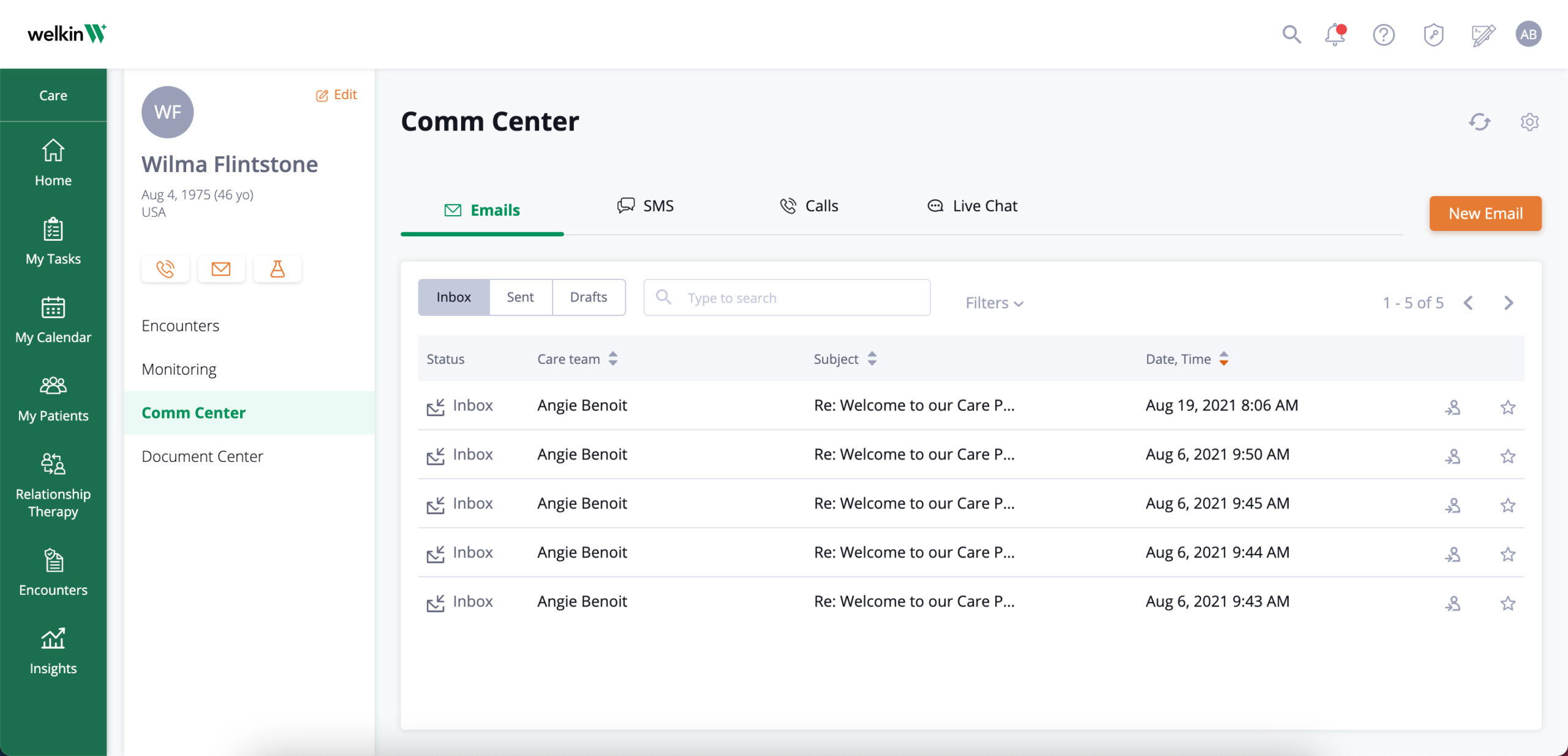
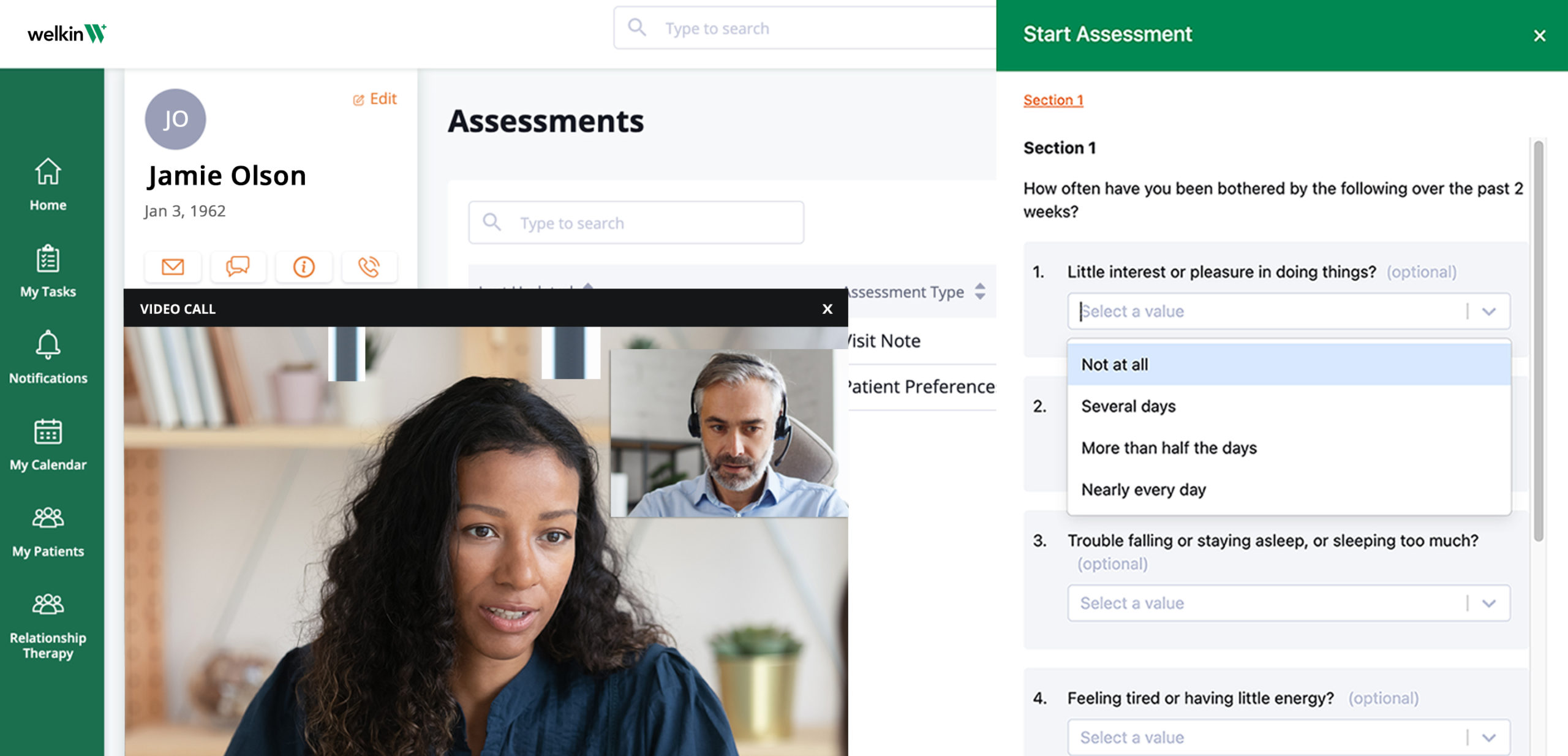
RPM encounter management:
Create and track all 6 RPM billing codes within encounters.
Features:
- Capturing the billing information needed for RPM including the CPT codes, ICD-10 billing codes, provider information and documentation required
- Encounters can include: appointment date, associated notes, clinical documentation, billing codes, disposition notes (date, note, time spent), and billing practitioner that visited with patient
- Audit log of all activity to support billing
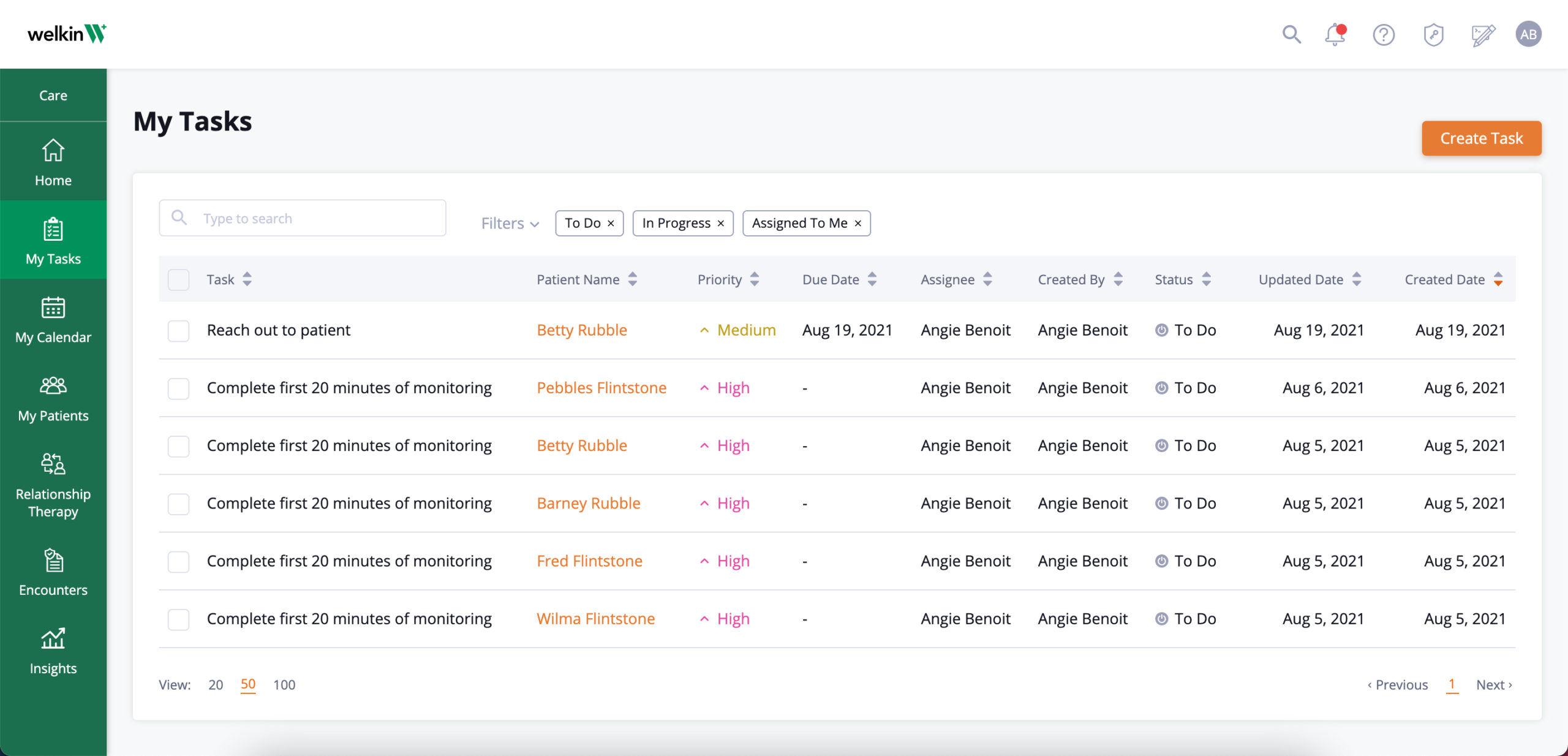
RPM program automation:
Automate care workflows to ensure patient is staying on track.
Features:
- Automate alerts to providers when a device reading is not within acceptable limits for immediate action
- Automate patient engagement including communication and assessments
- Push communication to your care team when an adverse event occurs
- Encourage compliant patients to continue their progress when positive outcomes have been achieved
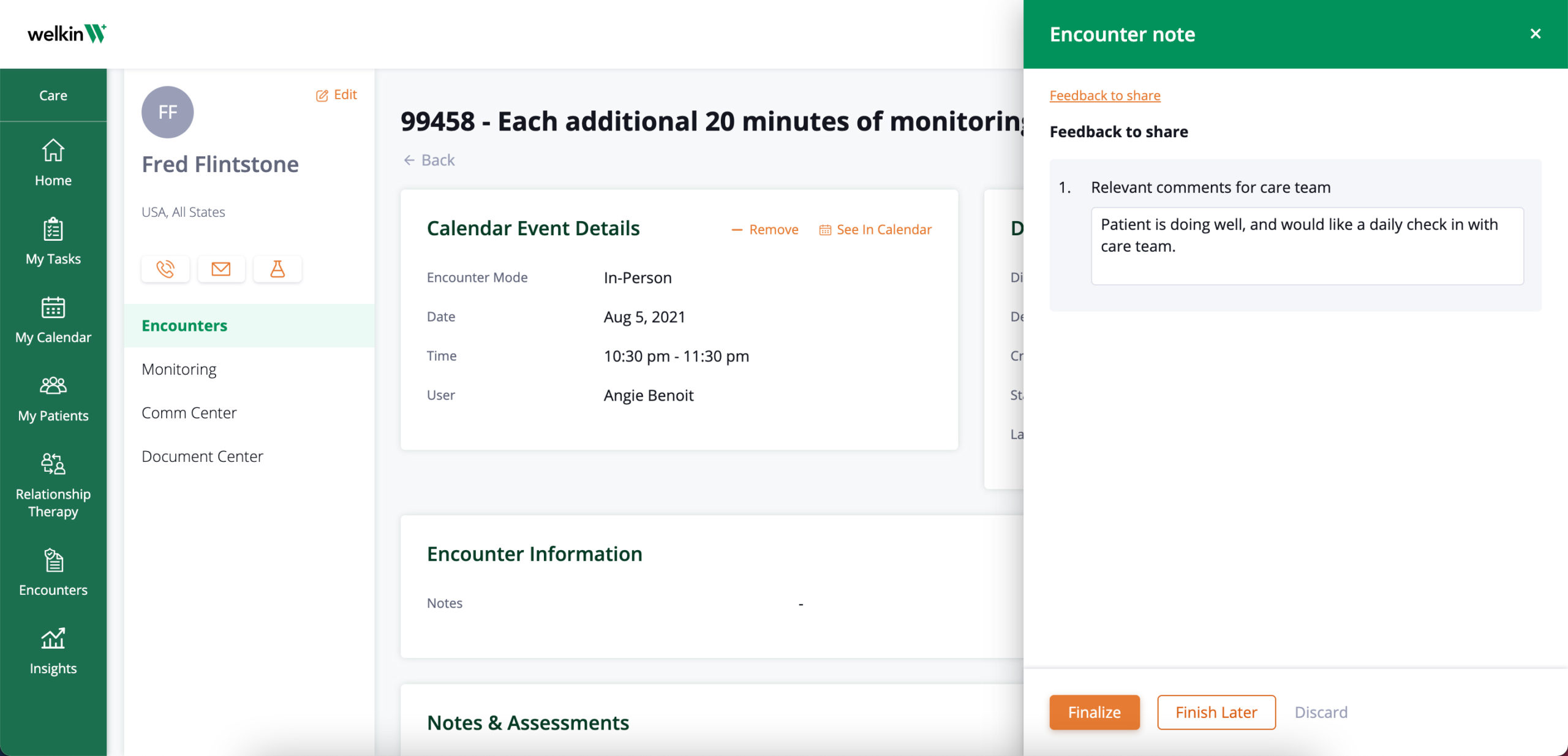
Accessible data:
All data is logged directly to a patient profile to track progress over time.
Features:
- Keep record of patient encounters, notes, assessments, and trending charts and graphs
- All data compiled is exportable to support your billing needs
- Download and export encounter reports to reference and share data outside of your organization
- Connect activities to appropriate billing codes so you can report out on the activities associated with each code

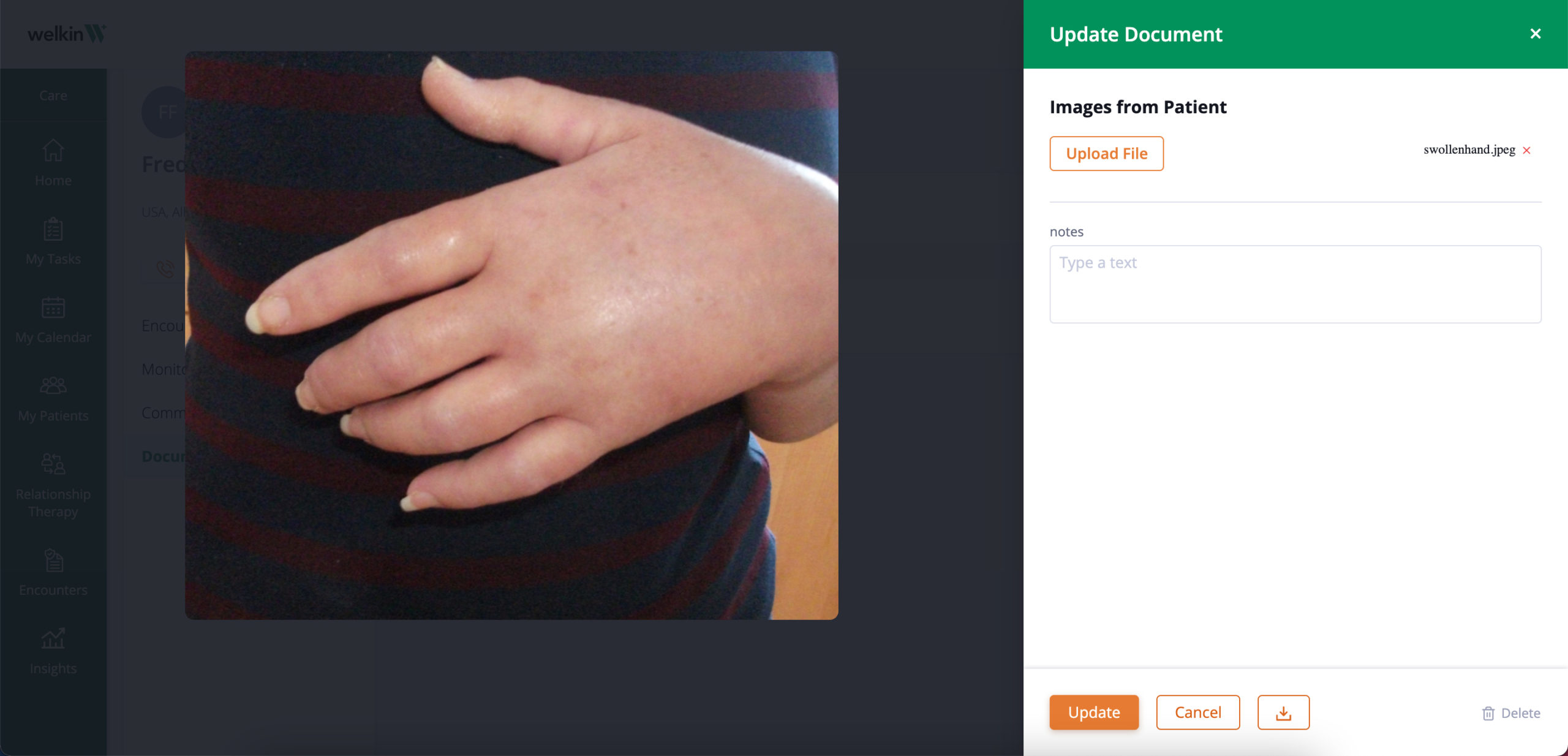
Monitor trends / trending data:
Sync patient information captured from the device to monitor trends over time.
Features:
- Visualize success or adverse events with charts & graphs on the patient profile
- Capture all vital data manually or via API

System flexibility:
Adhere to the ever-changing reimbursement definitions.
Features:
- Codeless program designer allows you to easily adjust care plans and programs easily
- Record all types of interactions so you can ensure reimbursements at all times
- Accommodate for your unique reimbursement model to get paid in the way that works best for you