Here’s a grim projection: by 2034, there won’t be enough doctors (estimates put this shortfall between 37.8K and 124K physicians). What happens to patients then?
There are no easy answers. And there is no single method or means of combating the consequences of this decline in available clinicians. It will take a multilayered approach to ensure patients get consistent, high-quality care in this new reality. But one key layer, one clear path in this approach, involves expanding the care circle beyond physicians by embracing a true care team model that’s supported by good, intuitive, useful automation. We need to facilitate a distributed care model where various care team members can support a patient with the right intervention or support at the right time in the patient journey, and leverage each team member’s unique skill set.
Here’s how automated technology and a balanced care team setup might play a crucial role in pulling patient care back from the brink.
Let physicians do what they do best
In a high-functioning care team model, although clinicians are kept up-to-date on care, they’re reserved for specific duties, the ones that only they are qualified to do (like diagnosing patients or prescribing a course of treatment). They’re not required to issue reminders, create a meal plan, check in with patients on routine matters, monitor blood pressure. Why? Other people on the care team are perfectly qualified to execute on those types of tasks, freeing the clinician to do what they do best without compromising standards or outcomes. When that happens, physicians can take on more patients while still delivering care they can be proud of.
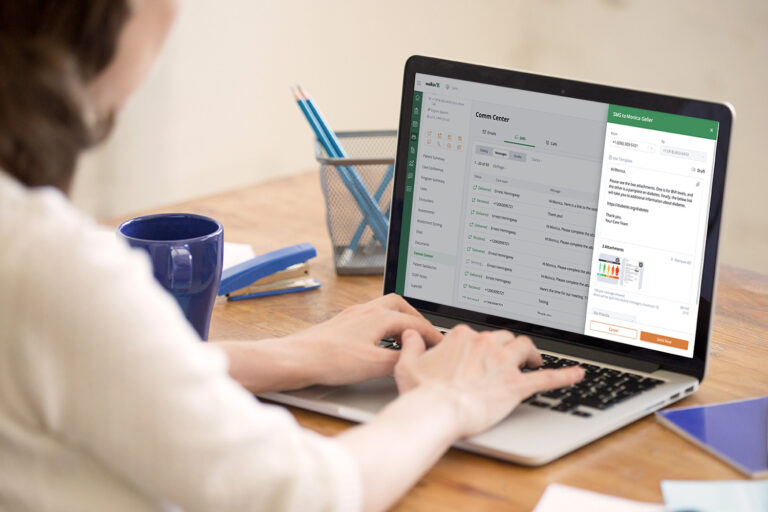
And automation in technology supports it. For example, perhaps a patient needs to have a specific treatment every three days, which necessitates some team follow-up. Automation provides a reliable nudge to ensure these tasks get done and alerts triggered by the system ensure physicians can provide oversight, particularly with high-risk cases, without getting too deep in the weeds. This is especially helpful with chronic conditions that require ongoing, high-touch efforts to keep patients compliant with treatment and on track — like diabetes or addiction recovery.
Play to human beings’ strengths
As a species, our memories are notoriously awful — particularly with multitasking, where studies have shown “we become less efficient and more likely to make a mistake.” That’s an obvious issue for clinicians, who see about 20 patients every day and work an average of 51 hours per week. Automation makes it possible to relieve the mental burden associated with the little, tedious and repetitive tasks that must get done but also pull focus away from patient care. This is critical: information overload is real and it degrades a caregiver’s ability to make good, measured decisions.
A system that includes intelligent, customizable, intuitive automation ensures that caregivers can double down on what they’re uniquely able to deliver: that human touch, the engagement with patients that helps reassure, drive consensus on treatment plans, and encourage compliance.
Identify ways to improve your care
Automating clinical workflows is a smart way to generate a data set that you can track, analyze, and ultimately use to understand the long-term progress of patients as well as the performance of the care team. Think about all the actions you could capture — for example, when outreach happened, the success or failure of a treatment plan, compliance with medication, patient response, test results, etc. — and how those could be evaluated to determine if a pivot is necessary. You would be able to move much faster to course correct.
You could even take it one step further. Automation makes it possible to do A/B testing — teams could try one configuration of automated tasks and workflows and contrast it with another. In the right system, this is easy: rules for automated tasks and triggers can be quickly created and changed. Running these experiments on parallel tracks makes it simple to see what’s working and what’s not.
Give what’s needed and nothing more
In automated systems, a robust rules engine enables a customized approach to patient care, which is crucial because, like physicians, patients are not immune to information overload. A one-size-fits-all style is a guaranteed path to communications and outreach that feels spammy and impersonal, a far cry from the tailored, hyper-personalized interactions patients are accustomed to in their consumer spaces. Such a process almost certainly contributes to lower patient satisfaction scores and does not drive the behaviors that positively influence good patient outcomes.
But imagine the difference when patients get precisely what’s needed for them as individuals. A robust rules engine drives that for care teams, ensuring that they have control down to fine-grained level — like stacking triggers (e.g., messages to patients go only at this specific point in treatment and only if they have these certain symptoms).
A best practice in healthcare should always prioritize relevance for patients as the default communications standard.
Have you used automation in your practice? How has it informed better patient care?
About the Author:
Michelle Pampin is the CEO of Welkin Health, a Care Management platform focused on improving health outcomes for people living with chronic diseases. Michelle is an accomplished leader, with a track record of advancing high-growth Silicon Valley software companies. Michelle speaks three languages: Spanish, French and Portuguese. When she’s not busy leading Welkin, she is busy staying active with her Samoyed, Avi.