As we get further into 2022, the writing on the wall is absolutely enormous: digital health is having more than a moment. It’s here for the long haul.
At the same time, in-person medicine will never go away. We all take comfort in seeing our doctors, there’s frequently a demonstrable need for it, and it’s how things have been done for centuries. This points to one inescapable conclusion: just like the future of work is hybrid, so too is the future of medicine, a world in which both care modalities co-exist and complement each other.
So in 2022, how will we see hybrid medicine – that flexible blend of telemedicine and in-person care – start to take meaningful shape?
Expect distributed care models to become the norm
88 percent of Americans have a chronic care condition, issues that necessitate astute and timely management. Now couple that with an imminent physician shortage (one estimate puts the shortfall as high as 134,000 doctors by 2034) and on the surface, you have a prescription for disaster. Too many patients who need care, not enough doctors to deliver.
But is it truly an issue – or do we just need to shift from our “doctor-first/doctor-for-everything” mentality? It’s really the latter. We should look at care as a true team sport, particularly in chronic care where frequent check-ins are non-negotiable to ensure patients stay relatively healthy.
In a distributed care model, the doctor is the quarterback whose time and talents are reserved for the moments when they can make the maximum impact. They’re called in for the difficult diagnoses, interpreting test results, setting a treatment plan, etc. But to have them monitoring blood pressure on a monthly basis, reminding patients to stick to their nutrition plans, sharing links to useful research or recommendations? No. Other care team members – nurses and nurse practitioners, physician assistants, dieticians, pharmacists, social workers, administrative staff – can pick up that work, freeing clinicians to provide the kind of patient care that only they can give. We see it daily with our customers where having one physician and 10 team members is rapidly becoming the de facto standard.
Watch for these “physician extenders,” already popular in emerging digital health models, to be initially embraced by many as a short-term solution to the physician shortage – but then find a permanent place because of the demonstrated value they deliver.
Value-based payments will take center stage
The distributed care model really gains momentum when a value-based payments model replaces fee-for-service. Why? The priority shifts from generating revenue from tests, appointments, referrals, procedures, etc., to being incentivized for keeping people healthy through proactive prevention and health education.
A distributed care model is better equipped for this. It’s deliberately architected so that more team members are focused on tracking and supporting every aspect of care precisely so patients can reach, maintain and extend their good health. Many digital health providers we speak with are leveraging value-based payments as we speak. Teams like Upswing are using technology and teams to ensure that only regular, reasonable and warranted check-ins and interventions take place to keep costs down, manage conditions in-house (versus expensive referrals) and, most crucially, drive positive patient outcomes.
Technology can make it all happen
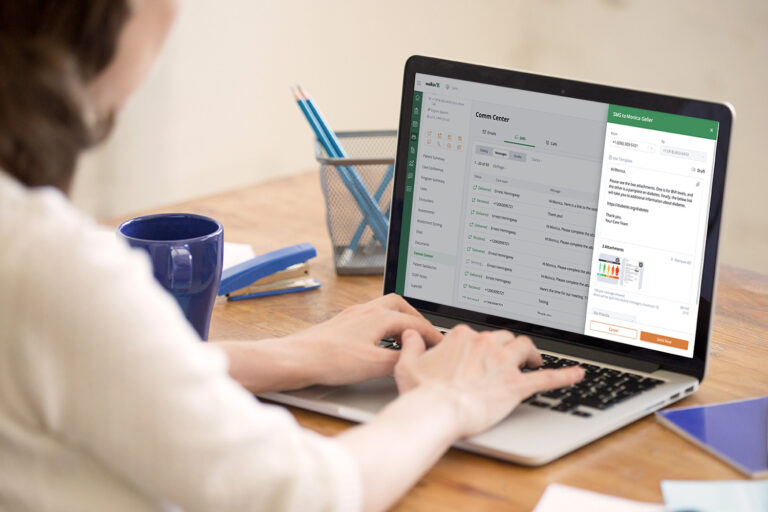
For the millions with a chronic care condition, the hybrid medicine model is best facilitated through technology. It supports the education, listening, reassurance, check-ins and as-needed in-person visits that help patients stay on track and successfully manage their health. Texts, emails, video conferences, etc, are all very simple, lightweight, low-cost and low staff time patient communication elements that can have an outsized impact. When combined with real-time alerts on test results, medication adherence, anomalies, etc, it gets a lot easier to achieve the type of preventive care that keeps people out of the hospital and the primary care office.
In other words, you’ll see technology work as a facilitator that prioritizes for care team members so they can focus on what’s important. Like a net, technology can help teams handle most issues that arise, ensuring that the complex anomalies best suited for humans are routed to them and everything else is rapidly handled.
What are your predictions for hybrid medicine in 2022?
About the Author:
Michelle Pampin is the CEO of Welkin Health, a Care Management platform focused on improving health outcomes for people living with chronic diseases. Michelle is an accomplished leader, with a track record of advancing high-growth Silicon Valley software companies. Michelle speaks three languages: Spanish, French and Portuguese. When she’s not busy leading Welkin, she is busy staying active with her Samoyed, Avi.