Comorbidities, conditions simultaneously present with another condition, have become a unique challenge to patients and care providers alike.
Comorbidities are often long-term and chronic. Common examples of comorbidities in the United States include:
- Arthritis
- Diabetes mellitus
- Hypertension
- Heart disease
- COPD
- Obesity
- Mood disorder
- Substance use disorder
Studies on COVID-19 are also showing a pattern of comorbidities that require further long-term research. The co-occurrence of these physical and mental disorders presents clinicians with concurrent monitoring and treatment challenges.
The increasing prevalence of comorbid conditions often complicates primary care health services—as it requires treatment and long term follow-up by a variety of specialists. Patient monitoring technology has helped both clinicians and public health officials treat and prevent many of our era’s common comorbidities.
A brief history
For centuries, healthcare providers diagnosed and treated health holistically—accessing and addressing the patient’s entire ecosystem to find the root cause of dysfunction. When modern science innovated diagnostic tools and therapeutic methods, clinicians began to target specific, isolated impairments in the body’s functions. They began to prioritize the pathogen or condition over the host and the host’s living environment.
These healthcare discoveries raised a question: how, and in which order should concurrent medical conditions be evaluated, diagnosed, and treated?
The answer came in 1970 when epidemiology researcher Alvan Feinstein was studying patients with rheumatic fever that were also diagnosed with other medical conditions. It was Feinstein who coined the term “comorbidity,” founding a new branch of medicine in the United States and developing new diagnostic guidelines for clinical practice.
Today, comorbidity care has become a critical avenue for the validation of medically unexplained health problems like headaches, pelvic pain, lower back pain, irritable bowel syndrome, fibromyalgia, and urinary tract symptoms, which often present as comorbid conditions.
Comorbidity prevalence in the U.S.
According to the American Journal of Preventive Medicine, comorbidities are highly prevalent among hypertensive adults—about a third of adults in the United States have hypertension. Most of them are also receiving treatment for other costly comorbid conditions, like heart disease and stroke.
A study published by The National Institutes of Health found that, after hypertension, the most common comorbid conditions in the United States are diabetes mellitus, respiratory disease, and pulmonary disease. The prevalence of comorbidities like these increases with age for both men and women. Conversely, the prevalence of substance use disorder and obesity decreases with age.
What are some common examples of comorbidities?
The Harvard School of Health reports that 70% of annual deaths in the United States are due to chronic diseases like heart disease, diabetes, cancer, and stroke—all of which are often associated with comorbidities.
According to the CDC, 1 in 10 people in the United States has diabetes. What many of them don’t know is that they may be at increased risk for other comorbidities. Here are some of the most common comorbid conditions that U.S. clinicians are currently treating and monitoring:
- Arthritis: this chronic condition commonly affects adults with other chronic conditions like diabetes, obesity, and heart disease. In fact, adults with these three chronic conditions are twice as likely to develop arthritis.
- Diabetes mellitus: excess glucose levels make it difficult for the pancreas to produce enough insulin. This chronic condition develops gradually—1 in 3 Americans have pre-diabetes—and can be controlled with diet and lifestyle changes.
- Heart disease: an umbrella term for those conditions that affect the heart—arrhythmia, cardiomyopathy, coronary artery disease, atherosclerosis, and congenital heart defects—which affect over 30 million people in the United States.
- High blood pressure: diet, lack of exercise, genetic predisposition, hormone imbalance, diabetes, and high cholesterol can all increase blood pressure to unhealthy levels.
- Psychiatric disorders: anxiety and depressive disorders often overlap. For example, a social anxiety disorder (SAD) diagnosis is often followed by a major depressive disorder (MDD) diagnosis in the same person.
- Substance use disorder: surveys conducted across the country have found that nearly half of people diagnosed with mental illnesses—like major depression, mood disorder, anxiety disorder, bipolar disorder, and personality disorder—also develop substance use disorder and vice versa.
Treatment challenges
Clinicians treating comorbidities face unique challenges. According to The Lancet Psychiatry Journal, this is often due to psychiatric risk factors. Patients with mental disorders may have trouble complying with medication protocols, complicating treatment and monitoring.
Emotional distress is also often elevated in people with chronic conditions. For instance, compared to the general population, people with diabetes are twice as likely to have depression. Mood regulation medication protocols for mental illness, however, may conflict with blood glucose regulation requirements and vice versa, negatively impacting the patient’s quality of life and potentially prompting contraindications.
When physical disease treatments and mood management can be integrated, and self-regulation—healthy eating, exercise, social-emotional health—promoted, synergistic mind-body healing becomes possible. This type of whole-person care requires consistent communication and diligent monitoring by a collaborative care team.
How to manage comorbidities
In the United States, 75% of health dollars go toward treating chronic conditions that have related comorbidities. Many of these dysfunctions can be managed with diet and lifestyle changes that drastically improve patients’ quality of life.
Historically, clinicians in the United States have focused on treating intense acute events—like respiratory distress, insulin shock, or anxiety attacks. Today, mainstream medicine is shifting into the preventive, integrative space.
Integrative medicine addresses the root cause of dysfunction and a wide range of environmental, social, physical, mental, emotional, and spiritual factors in a patient’s health. This model is proving to be effective in delivering whole-person care. Because comorbid conditions simultaneously affect multiple systems of the body—rather than just one system or organ at a time—their treatment must also nurture the whole patient.
Rather than waiting for these late-stage chronic disease episodes to land a patient in the emergency room, clinicians are honing in on risk factors early on.
By integrating a whole-person care approach, primary care providers and specialists are educating and teaching patients to self-monitor, communicate their symptoms, and share lifestyle change victories on a regular basis. When clinicians consistently communicate with their patients, they build trust, and patients begin to see them as consultants who care deeply about preventing chronic disease before it can disrupt their quality of life.
Monitoring indicators like blood pressure, blood glucose, diet, exercise, and social stimulation enables clinicians and patients to work together to prevent extreme episodes and unnerving, expensive trips to the ER or immediate care clinic—where treatment is only available from clinicians who aren’t familiar with the patient. Long-term relationships that build trust through consistent monitoring and education can help prevent comorbidities and create whole-person care success.
How does technology help treat and prevent comorbidities?
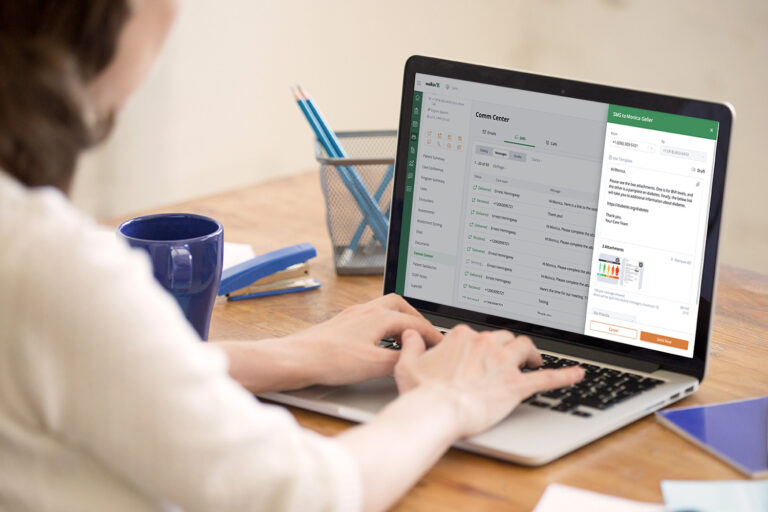
As the prevalence of comorbidity increases along with the practice of whole-person care in the United States, it’s becoming clear that preventive strategies and interventions will require more frequent and consistent real-time communication between patients and clinicians. It requires robust and effective Care Management—which is enabled by technology.
Care Management—all of the strategic clinical activities designed to educate patients so they self-manage their health conditions—improves patient care and outcomes.
This next-generation innovation reduces the need for medical care. It enhances care coordination by eliminating duplication and ensuring care team members are all on the same page. When the tracking and data entry responsibilities of clinicians are simplified or eliminated, they’re able to fully focus on improving their patients’ quality of life.
The right Care Management program has been shown to help care teams build more trusting, long term relationships with patients, who learn to not only comply with, but enjoy their more frequent touchpoints and friendly follow-ups. When they feel their clinicians truly care, patients report higher satisfaction, which gradually motivates healthier behavior, leading to improved clinical outcomes.
Care management technology can also help care teams reduce costs over time. Management programs that enable hospital-to-home transitions have been shown to reduce readmissions, which otherwise greatly increase health systems’ operational and facility costs. Care Management programs can also reduce the need for expensive acute care procedures and prevent the duplication of tests and specialized treatments.
When health systems reduce administrative tasks, they streamline care delivery, freeing up time for more meaningful interactions with patients. By saving time and energy, a quality, next-generation Care Management program can ultimately help you scale your organization and deliver higher quality care to more patients—every care manager’s dream.
To learn more about this promising trend, read our comprehensive guide to Care Management.