Anyone who’s ever had a sprained ankle, a broken wrist, a tweaked knee knows the frustration from what feels like it should be a fairly minor injury. Most of the time, that’s because the precipitating circumstances that caused these injuries were something of a fluke: you tripped off a curb, stepped wrong walking down the stairs, fell awkwardly playing catch with your kid. But bodies cause other problems too: maybe you’re an athlete dealing with tendonitis, a remote worker managing carpal tunnel or neck pain, or you struggle with arthritis as you age.
Inevitably, whether minor or major, these conditions end up with the inevitable MRI and consultation with the orthopedic surgeon.
How necessary are these visits, really? Turns out that technology has rendered this typical cycle unnecessary — and it’s also pointing the way to a new, more patient-centric mode of care for musculoskeletal ailments.
Telemedicine is a gamechanger
The pandemic was a proving ground for telemedicine across a number of specialties – and musculoskeletal was one of them. It might seem unintuitive – after all, don’t doctors need to physically see ailments of this sort to make an informed diagnosis? Actually, no. In one recent study, telemedicine visits sufficed for the overwhelming majority of patients; just 13.8 percent needed in-person referrals and telemedicine addressed the issues in 82.74 percent of cases. What’s more: patient satisfaction was incredibly high. Nearly 94 percent of patients surveyed said they’d return for another virtual consultation.
No more unnecessary tests
Coinciding with the realization that telemedicine is transformative for musculoskeletal is the understanding that common tests are frequently unnecessary. MRIs have been the reflexive go-to as a diagnostic tool for musculoskeletal injuries. But it turns out, they’re increasingly not required. These “scans are easily misinterpreted and can result in misdiagnoses leading to unnecessary or even harmful treatments.” Research is clearly showing that “MRI findings that previously were considered to be operative can improve with conservative management” – in other words, that physical therapy, self-managed regimens and other options produce equally good or better outcomes for patients.
This is good news when you consider that the US is the leader in the number of MRI units available, the sheer volume of MRIs performed, and the cost (which is 42 percent higher than the UK, for instance). Fewer unnecessary tests save money, time and can accelerate better patient outcomes.
A newer, more personalized world
What comes next when as many tests aren’t needed? The door opens to more specialized – even more personalized – rehab programs. New digital healthcare companies clearly see the opportunities here – and they’re using apps, personal coaching, and the latest research to help drive faster patient outcomes at less cost to patients and the system. After all, whether it’s a program designed for your particular issue or for you as a person, the process ensures that surgery isn’t the first option (unless it’s truly warranted).
Payers are pro new models and methods
Orthopedic surgeons are expensive – the specialty is one of the highest paid, just behind plastics, with an average annual salary of over $500K. Payers are increasingly interested in working with their members on new ways of obtaining the care they need. The added benefit of this transition means visits with these pricey specialists are reserved for the people who truly need them versus, well, everyone.
Practically, this could look like a triaged approach that’s real time and actionable so patients are quickly, even automatically, shifted into the right swim lanes. Imagine, for example, having to wait two months to see one of these specialists, only to be told what you need is physical therapy. That’s eight long weeks where you could have been doing that work and accelerating your healing – talk about wasted time. A triage model ensures patient needs are met expeditiously (and for less cost).
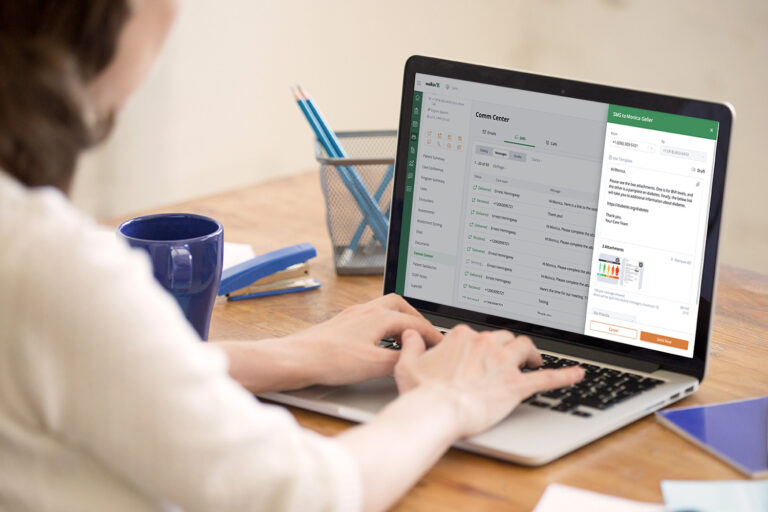
Technology platforms makes it all easier
Clinicians increasingly need more intuitive, responsive technology to manage hefty patient loads, ensure responsiveness, and improve outcomes. In musculoskeletal, a one-platform approach that can offer the care team the ability to design multiple pathways and programs is essential. The opportunity to create programs by factors like if an injury is acute or chronic, if it affects specific body parts, if it requires a low-touch or high-touch approach (or a mix of the two), is invaluable.
If you layer in the ability to securely check in with patients in multiple fashions (text, email, video, phone) along with automated alerts to ensure critical patient information (like test results) is elevated to the right team member immediately, it becomes much simpler to deliver a perfect blend of care. That means these established pathways and programs can be teed up – plus there’s additional flexibility to adjust, customize, and support unique patient needs in real time. What’s more: technology makes it possible to actually administer those rehab programs through those channels.
Additionally, patient contact and compliance gets easier. The success of most musculoskeletal rehab programs is consistency; it’s about doing what you’re supposed to do regularly. A platform can provide some essential services for top-notch rehab, including virtual assessments and healthcare touchpoints that enhance compliance. The ability to create automation, reminders and natural workflows make it simpler to check in with patients, establish and evaluate NPS scores, and deliver questionnaires like Patient Reported Outcomes.
Ultimately, technology is moving long-established medical specialties in the right direction – its transformative effect can cut down on cost, produce better patient outcomes, reorient the field away from unnecessary tests and referrals, and unite care teams in a more real-time, patient-centered approach.
It sounds like just the approach to embrace.