The Benefits of a Value-Based Care Model and How To Implement One
From technological advancements to the development of new treatment regimens, the healthcare sector is continuously seeking new ways to optimize patient outcomes. Digital transformation is revolutionizing the industry, and at the heart of shifting demands is the desire for personalized healthcare plans and experiences.
In recent years the focus of healthcare has shifted from a fee-for-service model to a value-based care model, which experts agree is better over all for the patient experience, as it increases patients’ engagement, reduces spending, and improves the organization’s reputation. It offers a more streamlined experience — as well as enhanced accessibility to information regarding a patient’s health — is helping drive patient engagement and health outcomes.
As a result, the healthcare space is adopting a more patient-centered approach. The advantages of implementing a value-based care model are hard to dispute — from promoting healthy habits and preventative care to decreasing costs and improving patients’ engagement.
What is value-based care in healthcare?
Value-based care is a delivery framework that incentivizes and reimburses providers based on the quality of care they provide patients. This model has emerged as an alternative to the traditional fee-for-service model as a way to put a patient’s best interests first and address their health-related needs in both the short and long term.
In a value-based healthcare model, wellness and prevention are embraced. Providers are directly rewarded for positive outcomes, which ensures the focus is rightfully placed on preventive care — reducing the need for costly tests, medications, and procedures. Focusing on dietary and lifestyle changes like quitting smoking and exercising, for example, can drive healthy habits and reduce healthcare costs for all parties involved.
Value-based care can help minimize complications and promote more effective disease management. This is due to the model’s integrated team approach, which shares patient data and coordinates care delivery to streamline intervention and better measure outcomes.
Let’s take a chronic condition like diabetes, for instance. In a value-based model, an integrated care team would consist of the patient’s primary doctor as well as supporting healthcare professionals to ensure the patient is maintaining a healthy diet and exercise regimen, dealing with the psychological facets of the disease, and keeping their blood sugar levels under control. This type of holistic care can effectively prevent problems entirely before they begin or stop them from snowballing into larger issues.
How is value-based care different from fee-for-service?
Transitioning to value-based care will require a recalibration of how payments are reimbursed and how quality of care is measured. In the traditional fee-for-service healthcare model, reimbursements are directly tied to the services a facility provides (i.e. more tests or services performed = more in billings for the organization). Unfortunately, this approach incentivizes the wrong behaviors, tying monetary rewards to the quantity of work performed.
In a value-based model, however, reimbursement is tethered to the efficacy of care provided along with positive patient outcomes. To put this into perspective, think about a patient visiting their primary care physician for a check-up and blood test. In this scenario, the fee-for-service approach would bill the patient solely for these services, treating it as a transaction with no added value in lieu of the level of care they received. In contrast, a value-based model would also take the outcome of the check-up and blood test into consideration. Did the patient get a diagnosis? Did they get better after treatment?
The fee-for-service model encourages providers and healthcare organizations to perform as many costly, high-tech procedures and fill as many beds as possible. This mentality only succeeds in driving up healthcare costs rather than emphasizing patient outcomes. Adopting a value-based care model, on the other hand, flips the script — putting the quality of patient outcomes first. By tying reimbursement to metrics surrounding outcomes, it’ll fundamentally pivot the focus of healthcare providers, ensuring patient needs are prioritized.
Government entities are pushing for a value-based healthcare model
Over the last decade, government-funded programs like the Centers for Medicare & Medicaid Services (CMS) have established a bevy of value-based healthcare models that focus on a pay-for-performance approach. Governments are supporting this model as it controls costs while increasing interoperability and improving health outcomes for populations as a whole. It should come as no surprise that there’s ample room for growth and forecasters anticipate a rising shift in government-backed programs and policies that support value-based care models.
The U.S. spends nearly two times more on healthcare than the average OECD country (which includes high-income nations like Germany, Australia, Canada, France, and the United Kingdom), yet we lag behind many countries on the same list in positive healthcare outcomes. From high chronic disease burdens to lower life expectancy rates, we have an opportunity to extract vital findings from care models outside the U.S. that focus on reducing costs without sacrificing quality.
Whether it’s packaging services — like a consultation, surgery, and physical therapy — to deliver more value, or embracing flexibility so more people invest in their own well-being, value-based care can help move the needle on healthcare reform.
The benefits of value-based care models
This proactive, patient-centered approach to healthcare has far-reaching benefits for all parties involved. Through a value-based care model, the health of our society as a collective will vastly improve over time.
Costs associated with managing chronic conditions would decrease, and the emphasis on preventive care would reduce the volume and frequency of medical emergencies and hospitalizations. When value and outcomes are prioritized over quantity, care delivery becomes more personal, holistic, and effective, leading to increased patient satisfaction and engagement.
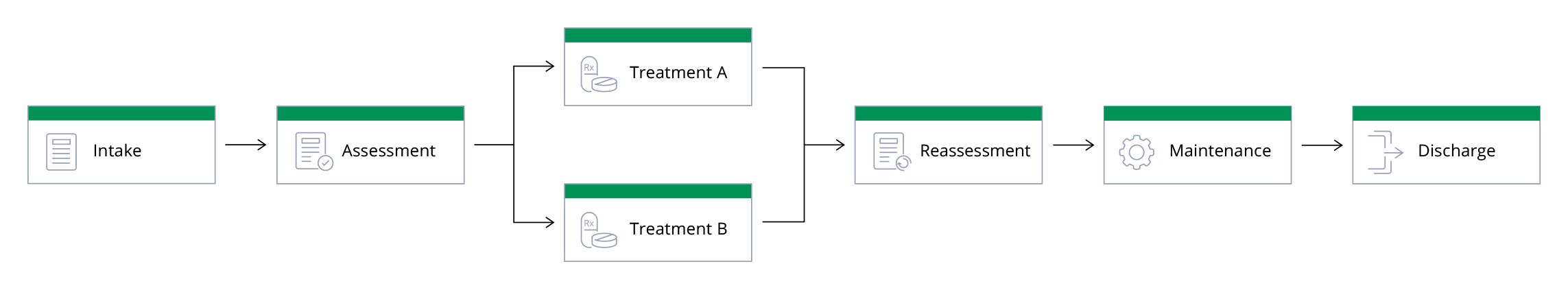
How to implement a value-based care model
As the healthcare industry shifts its focus from a fee-for-service framework to a value-based care model, some care providers — though eager to implement these changes — are stumped by exactly how to do so. Follow these calculated steps to bring value-based care to your own organization.
Organize care around patient conditions
According to Harvard University professor, Michael Porter, value creation occurs when a healthcare provider looks at a patient’s medical condition (or conditions), evaluates the potential outcomes and costs over the entire period of care for that condition, and implements an approach based on the patient’s individual health. Understanding your patient, their well-being, and their condition is the foundation of creating an effective value-based care model.
Measure patient outcomes and costs
Over time, trends that occur with patients who have the same condition can be analyzed to determine the best possible care plans and outcomes for that particular condition. In measuring the medical challenges these patients face and the associated costs of care, you can be better equipped to not only improve patient outcomes but also reduce the overall spending at your facility.
However, in order to track patient outcomes and costs, you must analyze your current (maybe outdated) measurement methods.
Outcome measurement
The first step to measuring outcomes is to define exactly what you are measuring and who the necessary stakeholders are when treating that condition (including the patient). Then, you need to put together a multidisciplinary team that will treat and care for the patient over the course of their condition’s cycle. If this seems like a daunting task, start with the Standard Sets outlined by the International Consortium for Health Outcomes Measurement (ICHOM).
Formed in 2012 by thought leaders from Harvard Business School, Boston Consulting Group, and the Karolinska Institute, ICHOM has brought clinical leaders and patients together — not just from the United States, but across the globe — to create outcome measure sets for 25 different conditions. These Standard Sets include everything from more common conditions like depression, anxiety, and lower back pain to genetic and rare conditions like congenital upper limb anomalies and craniofacial microsomia.
Once you have established your own outcome measurement sets, you can begin implementing your organization’s value-based care models and collecting data to further improve your individual care plans. This dedication to your patient’s well-being will be obvious to them, to your coworkers, and to the general public. In addition to improved patient satisfaction and patient outcomes, you can expect to build a reputation as a passionate group of care providers who truly care about their patients.
Cost measurement
Archaic methods of healthcare accounting systems rely on individual charges for tests, treatments, and consultations. When using today’s modern value-based care models, those systems prove to be inaccurate.
Time-driven activity-based costing (TDABC), an accounting concept introduced to healthcare by Harvard Business School professor Robert Kaplan in 2010, is one cost measurement method that analyzes cost by patient and condition over the entire cycle of care. TDABC creates incredible opportunities to improve efficiency and guide reimbursement.
To create a cost measurement system for your organization, you can begin by outlining all essential processes for treating a patient who has a certain condition — including personnel, equipment, space, and time. These factors will guide your cost measurement over time to determine exactly how much it will take to treat one patient for their condition over the course of the value-based care model.
Move to value-based payment
The current fee-for-service reimbursement model rewards healthcare organizations that value volume over quality of care. For this reason, two new value-based payment models are emerging.
Capitation
With a capitation payment system, a care provider or hospital is paid a fixed amount per patient for a certain amount of time by an insurer or physician association (IPA). Care providers contracted by an IPA can benefit from capitation for the following reasons:
- There are fewer billing staff on payroll.
- They won’t have to wait to be reimbursed for services.
- Alleviated costs and hassles allow their practice to treat more patients at a lower overall operating expense.
Bundled Payment
Bundled payments predetermine the total allowable acute and/or post-acute expenditures for an episode of care. With bundled payments, the care provider absorbs the costs that exceed this target price, but also reap the savings if they are able to spend below the target price while still maintaining quality.
These value-based payments align reimbursement with value — which, in turn, creates better patient outcomes. And with better patient outcomes, providers ultimately reduce spending and receive more patients due to their improved reputation.
Integrate care
When evaluating a network of healthcare facilities with multiple locations, it’s important to determine how you can deliver the right care in the right location to optimize the volume and capabilities of each facility.
To do this, you must take a hard look at how each location within your healthcare organization contributes to the network as a whole.
Four levels of provider system integration
According to Professor Michael E. Porter at Harvard Business School, there are four levels of integration for care provider systems:
- Define the overall scope of services. This will be determined by the location at which a care provider can best achieve high value for their patients, depending on different conditions and needs.
- Concentrate volume in fewer locations. By specializing locations to treat specific conditions, you can disperse the volume of patients and designate a higher volume of patients to the locations that can most easily treat that volume of patients — such as downtown facilities that specialize in common but difficult treatments like surgery and chemotherapy.
- Choose the right location for each service. You can decide this based upon the medical condition, acuity level, resource intensity, cost level, and need for convenience.
- Integrate care across appropriate locations. Care should be organized into integrated practice units (IPUs) around patient medical conditions.
The purpose of this structure is to deliver the right care at the right time in the right location so that your care team is trained to do what they do best, and patients will see the best possible outcomes — no matter which facility they visit.
Use technology
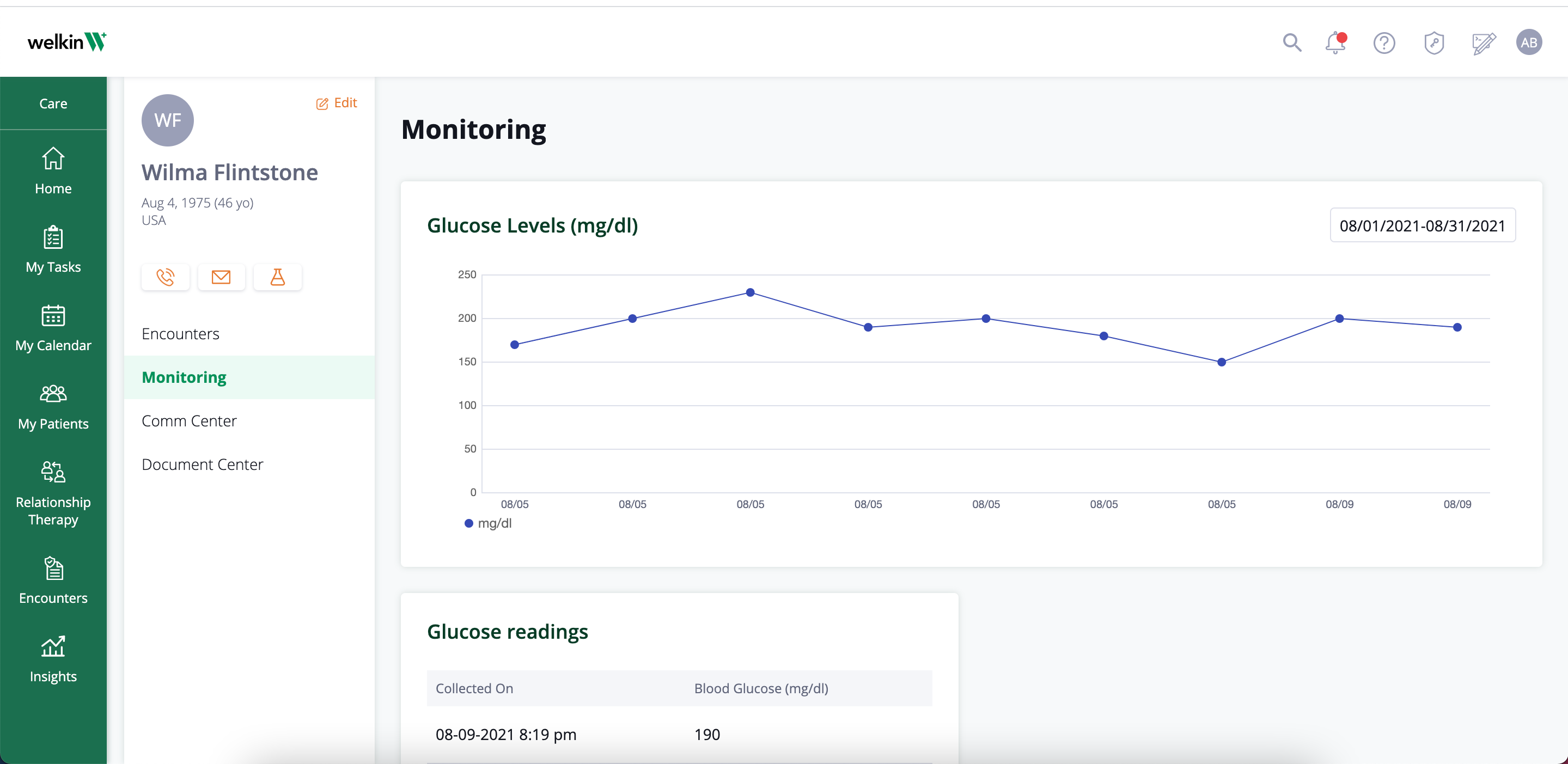
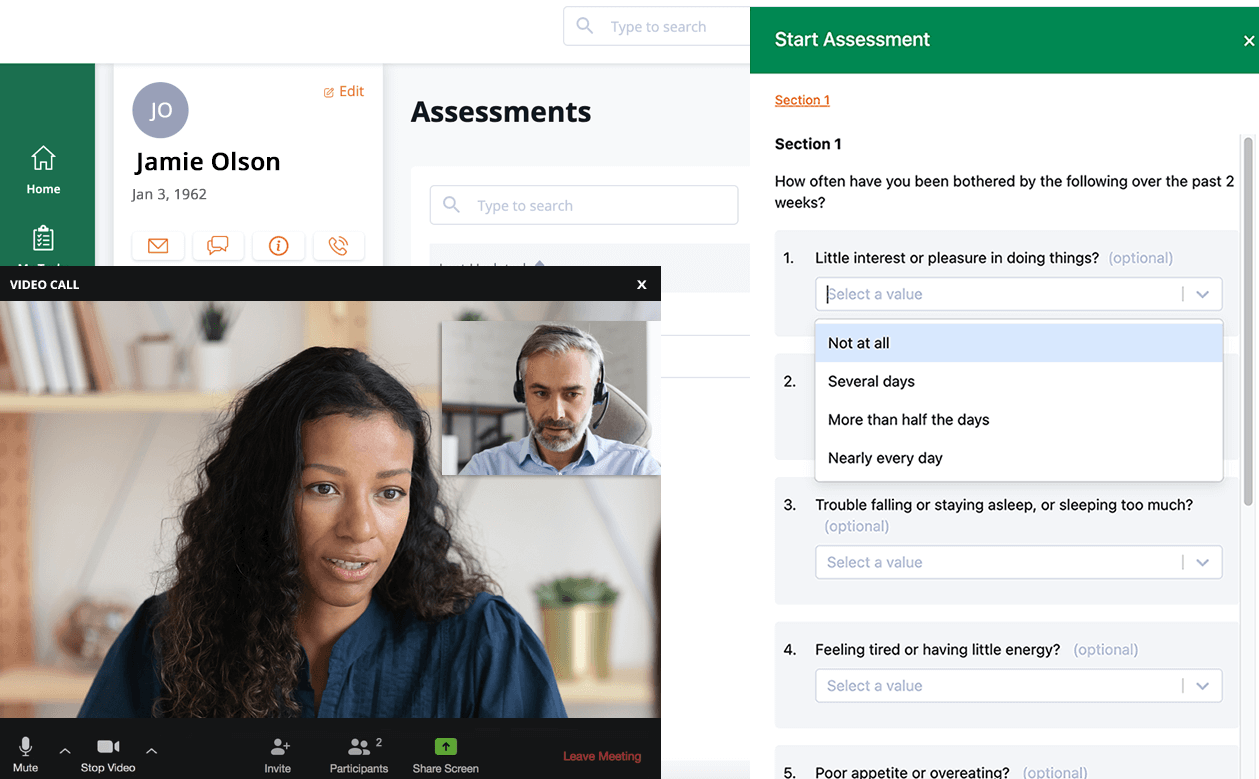
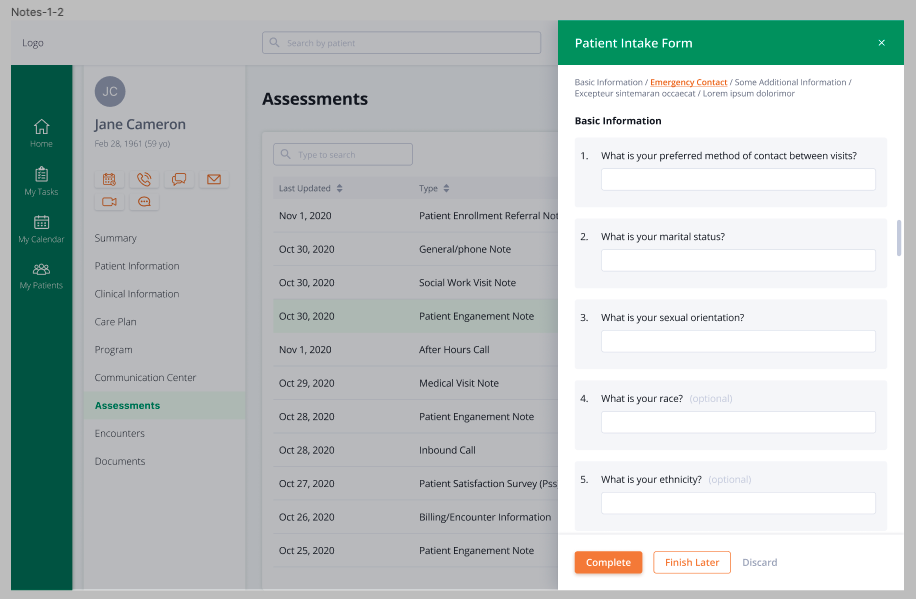
Technology is an incredible tool to support the value-based care model. It helps care providers deliver more positive health outcomes for patients through flexible, personalized program design. Integrated digital systems help clinicians easily understand their patient’s overall health, address patients’ care during and between visits, have all data and tools in one place, provide a more holistic view of each patient, offer patients different communication channels to choose from, and assess for social determinants to ensure patients get the care they need.
Using a good care management software will have a proactive approach to health while decreasing cost and hospital readmissions.
Start introducing value-based care models to your organization today
As you’ve seen, making the transition to value-based care models requires a lot of time, dedication, and resources. But the long-term sustainable success of your healthcare organization — plus the ongoing well-being of your patients and community — is well worth the effort of the shift.
For more information on how to start the transformation to value-based care at your organization, download our e-book How to Deliver Value-Based Care.
Example of value-based care program
Welkin Health: building blocks for more favorable outcomes
Software that can help your team shift to value-based care. Keep your members healthy – and your team ahead of the curve.
Increase Positive Outcomes
Increase your level of service by supporting your evidence based programs. Execute more efficiently against programs that are working through flexible program building and seamless communication with your patients. Effectively address patients that need care most during and between visits. Technology helps healthcare systems deliver more positive health outcomes for patients through flexible, personalized program design.
Get the Whole Picture
Make your team’s workload easier by getting a more holistic view of each patient – house all content, communications and data in one place. We even connect with external devices and applications to gain accurate insights into a patient’s health to detect any issues that might require extra support or immediate attention.
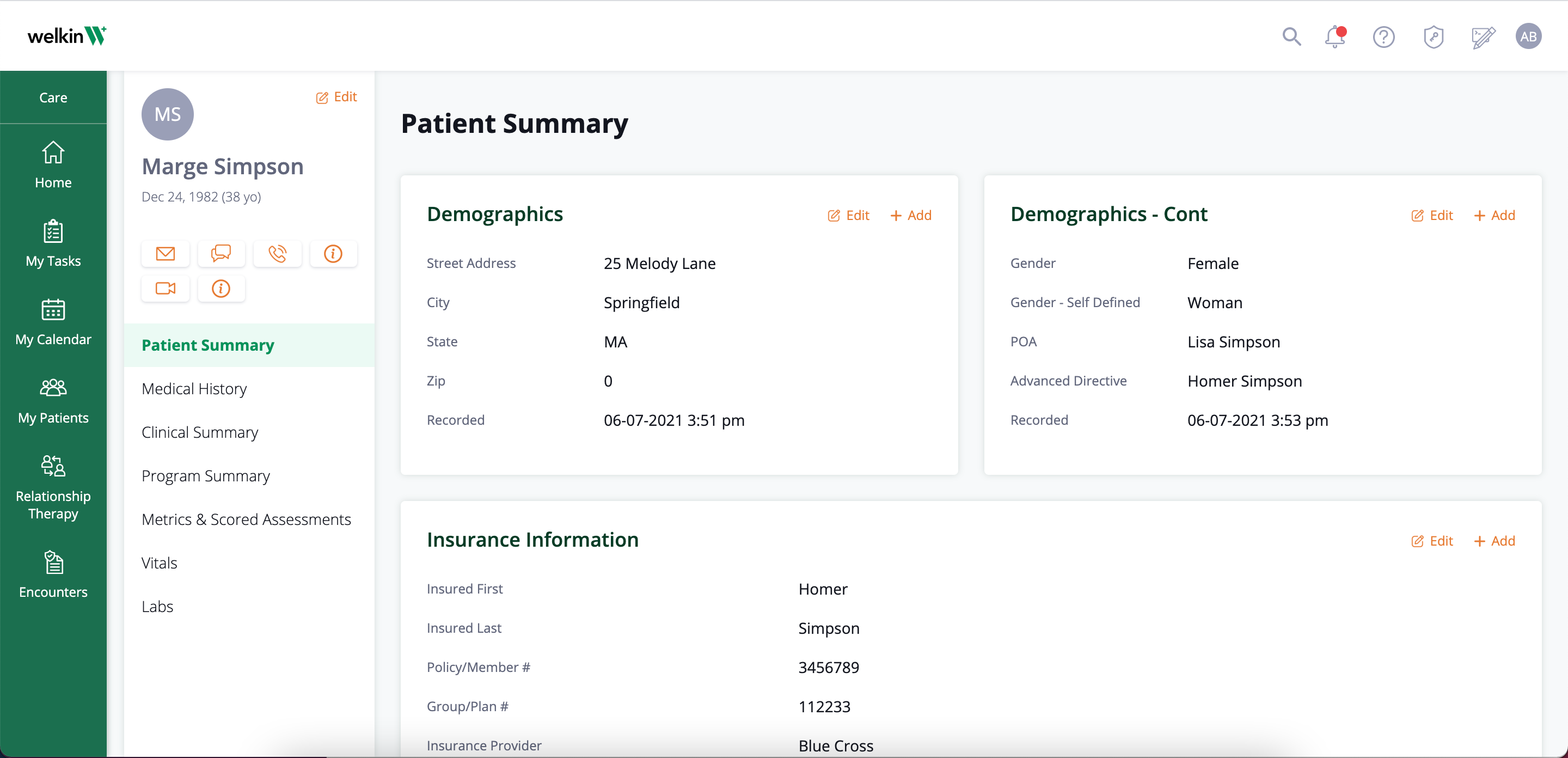
Address Social Determinants of Health
Achieve greater value through your value-based care program by addressing the social determinants of health. Welkin can help you assess for social determinants to identify patients that are at a higher risk of disease complications and ensure they get the care they need through additional services.
Engage Patients
With Welkin, providers can educate and encourage patients to become active participants in their wellness. In addition to keeping patients healthy, a proactive approach can decrease the risk and healthcare cost interventions and hospital readmissions. Studies show that patients who are satisfied with their quality of care are more likely to be compliant with treatment.
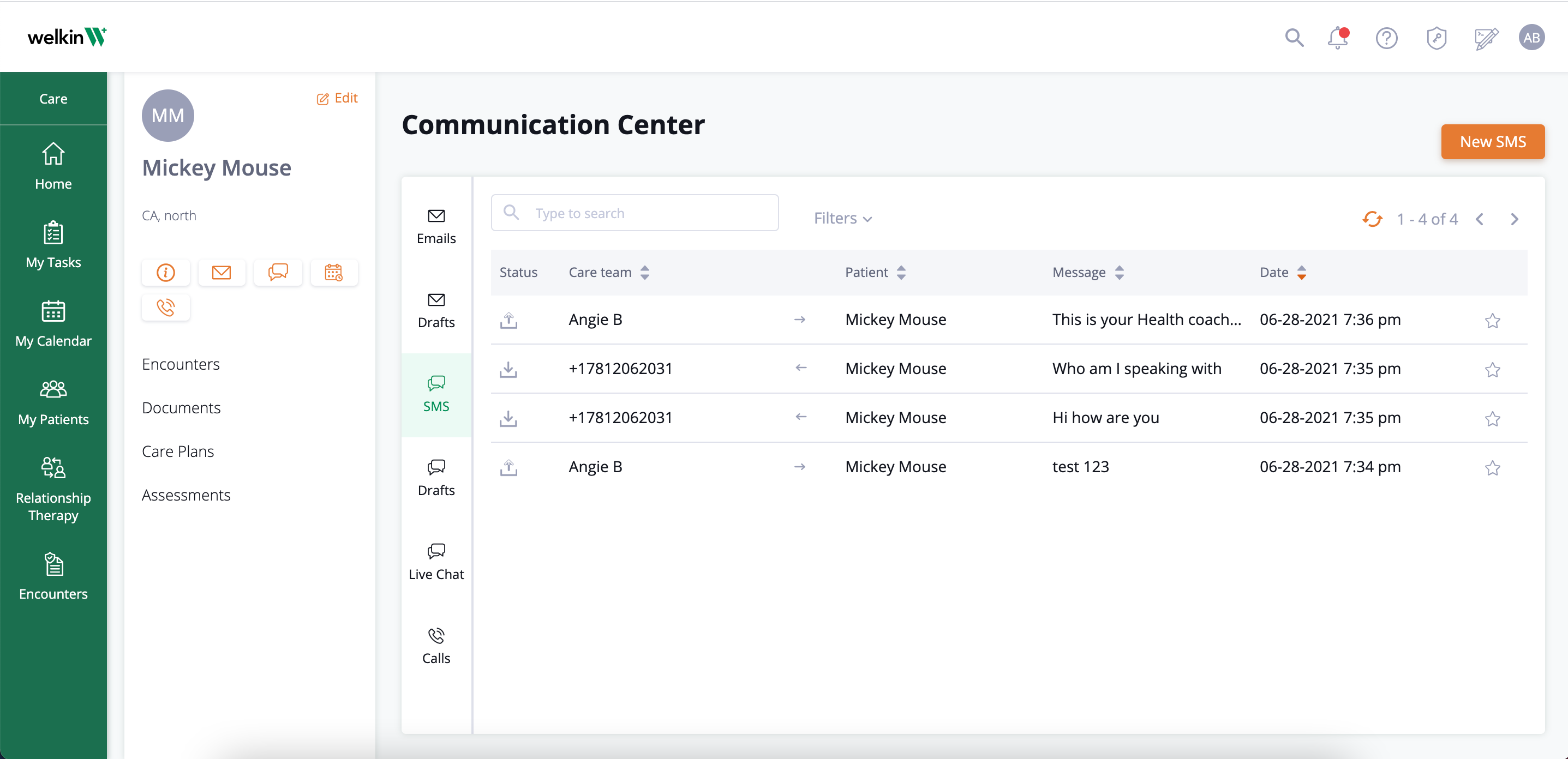
Streamline Communication
Good Care Management software will include multiple communication channels so you can connect with your patients on the platforms they like to use—email, text, phone, video, and app messaging. This makes it easy for the patient to reach out and won’t require you to invest in additional communications or plugins. A value-based healthcare system is one that focuses on health outcomes and helping patients thrive.
Spend More Time Caring for Patients
With Welkin, our simple platform enables your care team to centralize all the tools you need in one place, so that you can make care your number one priority. Value-based care models create a lasting doctor-patient relationship that benefits both you and the patients you treat. This model focuses on understanding what the patient needs for both their short-term and long-term health, and results in increased engagement and patient satisfaction, improved patient outcomes, and reduced costs.
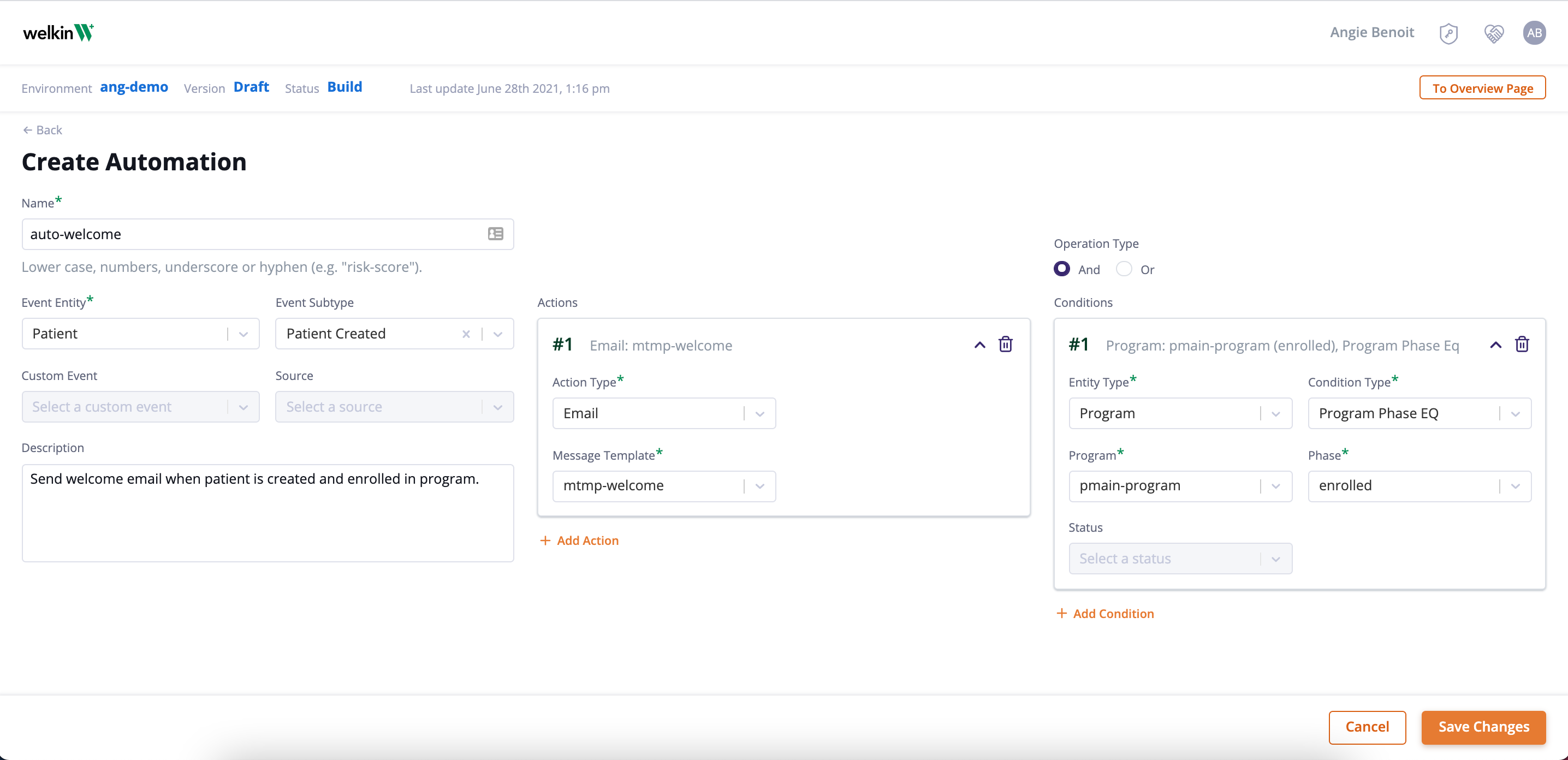
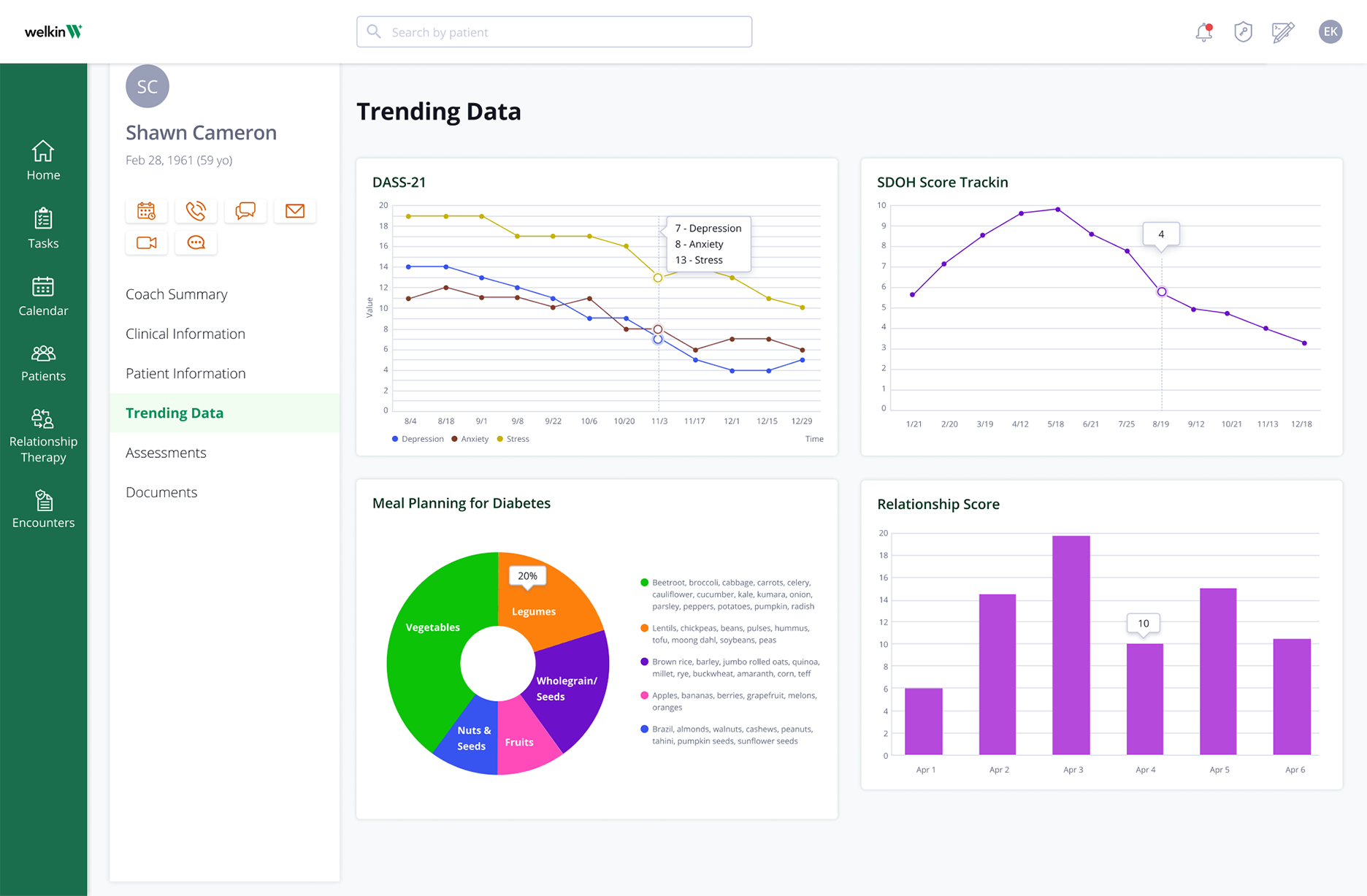
Prove your value-based program works
Healthcare professionals agree that providing value-based care is not only optimal for the patient experience, but it also improves an organization’s reputation and reduces overall spending. Technology is an incredible tool to support the value-based care model. Integrated digital systems help clinicians easily understand their patient’s overall health, communicate with their peers, and reach out to their patients when needed.